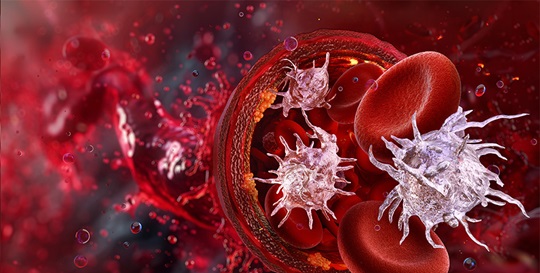
Thrombocytopenia is considered to be one of the most common causes of abnormal bleeding and bruising in the clinical setting. As there are many underlying mechanisms that result in thrombocytopenia, clinicians need to decipher whether it is caused by decreased production (inherited or acquired) or increased destruction due to immune processes, drugs, or consumption coagulopathies, for example.
A low platelet count is more than just a number—it’s a clue to an underlying cause that must be identified for effective treatment. Laboratories play a key role in supporting these decisions. They rely on diagnostic parameters that deliver clear, actionable insights while also fitting seamlessly into high-volume, cost-conscious workflows. Two key parameters that can help are the Immature Platelet Fraction (IPF) and Mean Platelet Volume (MPV), each with advantages and limitations. In this blog, we explore how they compare in supporting effective, efficient thrombocytopenia diagnosis.
Assessing Thrombopoiesis: Considerations for IPF and MPV
Labs face constant pressure to deliver accurate, timely results while managing costs and staffing constraints. Parameters such as the Immature Platelet Fraction (IPF) can provide valuable insight into platelet production. However, adopting IPF may involve additional workflow steps, require specialized reagents, and increase overall costs; factors that can be challenging for high-volume settings focused on streamlined operations.1
In contrast, Mean Platelet Volume (MPV) provides essential information on platelet size and production as part of every complete blood count (CBC). It is automatically reported on most hematology analyzers without the need for additional reagents, modes, or manual review steps. This built-in availability helps labs maintain consistent, reliable platelet assessment and simplifies daily workflows. MPV is also supported by extensive published research, reinforcing confidence in its value for routine use.2
Clinical Applications Where MPV Adds Value
MPV has demonstrated clinical value in multiple diagnostic contexts:
- Differential diagnosis of thrombocytopenia: In 2005, Bowles et. al published findings showing that mean platelet volume (MPV), measured on a Beckman Coulter automated analyzer, may provide clinicians with valuable information about the possible origin of the thrombocytopenia.3 This was the first paper to study the diagnostic predictive value of MPV. Using a dataset of 473 unselected patients with thrombocytopenia, they found that MPV can strongly guide clinicians as to the likely presence or absence of bone marrow disease in thrombocytopenic patients, thus differentiating hypoproductive thrombocytopenia from hyperdestructive thrombocytopenia. A 2023 meta-analysis showed MPV can also help differentiate immune thrombocytopenic purpura (ITP) from hypo-productive thrombocytopenia with 76% sensitivity and 79% specificity.4
- Risk assessment in cardiovascular disease: MPV predicts in-hospital mortality in acute coronary syndrome patients.5
- Monitoring bone marrow recovery: Studies show that MPV trends can help track remission in leukemia patients following chemotherapy or hematopoietic stem cell transplantation.5,6,7
These applications highlight MPV’s role in supporting sound clinical decision-making without requiring additional testing complexity or cost. It also integrates seamlessly into routine laboratory testing.
Complementary Roles for IPF and MPV
While MPV is often viewed as a more established parameter, evidence shows both MPV and IPF can offer valuable, complementary insights in appropriate clinical settings. For example:
- Rauf et al. (2023): In patients with non-ST-segment elevation myocardial infarction (NSTEMI), both IPF and MPV were significantly associated with left anterior descending artery involvement. Although IPF showed slightly better diagnostic performance (AUROC 0.738 vs. 0.674), both provided valuable clinical information.8
- Huang et al. (2019): IPF and MPV values were both elevated in acute coronary syndrome patients compared to non-ACS patients, highlighting their shared utility in assessing platelet activation.9
- Cesari et al. (2014): In BCR-ABL-negative myeloproliferative neoplasms, both parameters proved useful as markers of platelet activation and thrombotic risk.10
The Beckman Coulter Advantage
Beckman Coulter’s DxH 900 and DxH 690T analyzers are engineered to deliver high-confidence results, supporting faster clinical decisions and providing confidence for smear reviews. MPV is automatically and accurately reported, even in thrombocytopenic samples, ensuring labs get reliable platelet metrics without requiring additional modes, reagents, or manual steps. MPV is just one example of how Beckman Coulter delivers best-in-class hematology technology that supports clinical excellence and operational efficiency. With integrated, intelligent features designed to optimize workflow, reduce costs, and increase reportable results, DxH analyzers empower labs to streamline operations without sacrificing diagnostic insight.
Conclusion
Parameters like IPF can provide insight into platelet production, but often involve added steps, specialized reagents, and higher costs, which are important considerations for high-volume labs aiming to maintain streamlined processes. MPV can be a reliable alternative that offers crucial platelet information as part of routine CBC testing without adding complexity. Backed by extensive research, MPV helps laboratories deliver accurate diagnoses efficiently and maintain consistent, high-quality patient care.

 English
English