Diagnosing Alzheimer’s Disease
Early diagnosis and intervention can help to improve outcomes for individuals living with Alzheimer’s disease, as well as for their caregivers and families. Currently, the diagnosis of Alzheimer’s disease is made following subjective symptom reporting, cognitive testing, and a series of lab tests that rule out reversible or treatable conditions that can cause cognitive changes. Other testing includes imaging studies such as computerized tomography (CT) scans, magnetic resonance imaging (MRI), and/or positron emission tomography (PET) scans. However, changes in the brain may occur long before clinical symptoms are detected, making early diagnosis of Alzheimer’s disease particularly challenging. Alzheimer’s disease progresses on a spectrum of 3 phases: preclinical, mild cognitive impairment, and then dementia, which is further stratified into mild, moderate, and severe stages. How quickly patients progress through the continuum varies and is influenced by factors including age, environmental factors, genetics, and sex.1
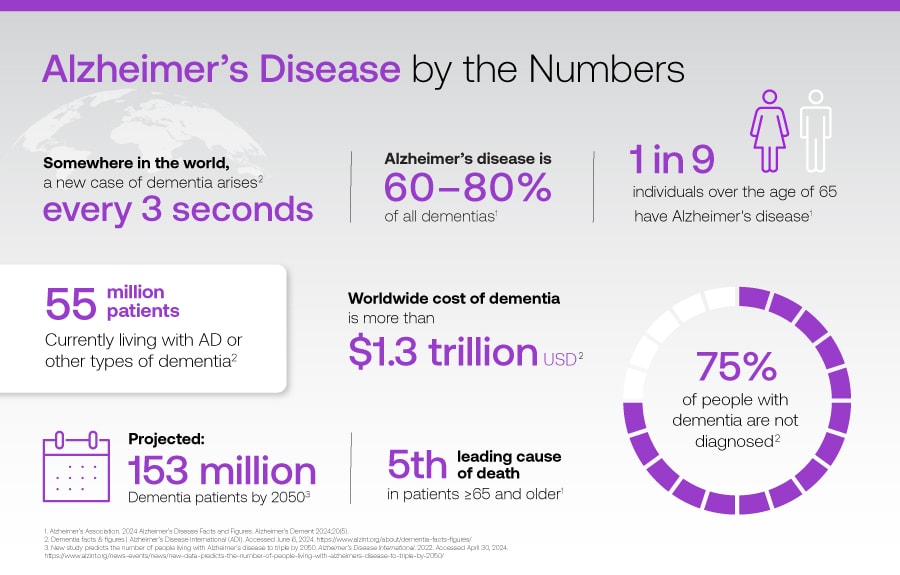
Download Alzheimer’s disease facts infographic ›
Diagnosing Alzheimer’s disease can be challenging for several reasons:
- Lack of definitive diagnostic tests: Currently, there is no single test that can definitively diagnose Alzheimer’s disease. Diagnosis is often based on a combination of medical history, cognitive assessments, and ruling out other possible causes of symptoms. While cognitive tests play a crucial role in the assessment and diagnosis of Alzheimer’s disease, they also have several limitations such as subjective bias, educational and cultural biases, lack of sensitivity and specificity, and variability in performance.
- Access to healthcare: Limited access to healthcare services can also be a barrier to timely diagnosis of Alzheimer’s disease. This can result in delays in receiving appropriate care and support.
- Stigma and denial: There can be stigma associated with a diagnosis of Alzheimer’s disease, which may make individuals hesitant to seek a diagnosis or share their symptoms with healthcare providers. Additionally, denial of symptoms by the individual or their family members can delay the diagnosis and appropriate interventions.
- Similar symptoms: The symptoms of Alzheimer’s disease can be similar to other conditions, such as other types of dementia or age-related cognitive decline. This makes it difficult to accurately diagnose Alzheimer’s disease, especially in the early stages.
- Variability of symptoms: Alzheimer’s disease can present differently in different individuals, with symptoms and disease progression varying widely. This variability can make it challenging to diagnose Alzheimer’s disease accurately and in a timely manner.
- Overlapping conditions: Alzheimer’s disease can coexist with other medical conditions, such as vascular dementia or Parkinson's disease (PD), which can complicate the diagnostic process.
Overall, diagnosing Alzheimer’s disease requires a comprehensive evaluation by a healthcare professional. The evaluation includes cognitive assessments, medical history, and sometimes imaging tests. Early detection and diagnosis are crucial for initiating appropriate treatments and interventions to help manage symptoms and improve quality of life for individuals living with Alzheimer’s disease.
Current Alzheimer's Treatment Options
The current treatment landscape for Alzheimer's disease includes a combination of pharmacological and non-pharmacological interventions aimed at managing symptoms and improving patient quality of life. Pharmacological treatments for Alzheimer's disease typically involve the use of medications that target cognitive symptoms, such as cholinesterase inhibitors (e.g., donepezil, rivastigmine, galantamine) and NMDA receptor antagonists (e.g., memantine). These medications can help improve cognitive function, behavior, and activities of daily living for some patients with Alzheimer’s disease. Non-pharmacological interventions for Alzheimer’s disease include cognitive stimulation therapy, physical exercise, and occupational therapy.
In recent years, there has been a growing focus on developing disease-modifying treatments (DMTs) for Alzheimer’s disease that target the underlying pathology of the disease, such as amyloid plaques and tau tangles.3 These treatments aim to slow or halt the progression of the disease, rather than just managing Alzheimer’s disease symptomatically.
Some of the emerging disease-modifying treatments for Alzheimer’s disease include:
- Anti-amyloid therapies: These treatments aim to reduce the accumulation of amyloid plaques in the brain, which are a hallmark feature of Alzheimer’s disease. Several anti-amyloid therapies are currently in clinical trials, including monoclonal antibodies that target amyloid beta proteins and beta-secretase inhibitors that prevent the formation of amyloid plaques.
- Anti-tau therapies: Tau tangles are another pathological hallmark of Alzheimer’s disease, and targeting tau pathology is another promising approach for disease modification. Anti-tau therapies in development include tau aggregation inhibitors and tau immunotherapy.
- Anti-inflammatory therapies: Inflammation is believed to play a role in the progression of Alzheimer’s disease, and some emerging treatments aim to reduce neuroinflammation and protect against neuronal damage.
- Combination therapies: Emerging research is exploring the potential benefits of combining DMT treatments to target multiple pathological mechanisms of Alzheimer’s disease simultaneously. These combination therapies may have synergistic effects and improve treatment outcomes.
After almost two decades of intense drug development efforts with several failed candidate drugs and clinical trials, recent progress has been made with the development and approval of two DMTs and symptomatic treatments for neuropsychiatric syndromes of Alzheimer’s disease. Three exciting new anti-amyloid treatments have been recently approved by the FDA for slowing the progression of AD.4,5,6 Brexpiprazole is another molecule that has recently received approval for the treatment of agitation in dementia associated with Alzheimer’s disease.7 These successes have been influential for Alzheimer’s disease therapeutics and demonstrate the ability to slow disease progression through intervention in key pathological processes of Alzheimer’s disease. The success of these molecules also firmly establishes the need for Alzheimer’s disease biomarkers both for diagnosing Alzheimer’s disease and as a means of following therapeutic responses. The approval of these recent DMTs also highlights an urgent need for improved diagnostic methods and the need for diagnosing Alzheimer’s disease in the earlier stages of the disease.
Overall, the emerging and rapidly evolving treatment landscape of Alzheimer's disease with disease-modifying treatments holds promise for potentially changing the course of the disease and improving long term outcomes for patients.
Our Commitment to Diagnostic Testing
Beckman Coulter and its proven high-sensitivity immunoassay capabilities are empowering healthcare providers, research organizations, and laboratories to address emerging diagnostic challenges across diverse specialties, from infectious diseases and neurological diseases to reproductive health. We are revolutionizing the next generation of specialized diagnostics through high-sensitivity immunoassays, driving innovation, advancing medical insights, and enhancing diagnostic availability and adaptability to better serve patients in a variety of disease states.
Learn more about Beckman Coulter’s commitment to neurological disease biomarker research

 English
English





