In addition to the human toll, sepsis is costly to healthcare organizations. Sepsis-related costs—which may include longer hospital stays, ICU admissions, hospital readmissions and extensive testing and patient monitoring—surpass $24 billion.6
The facts about sepsis
- 1.7 million people are diagnosed with sepsis each year in the U.S.
- 2/3 of septic patients enter the health system via the ED
- Sepsis is the No. 1 cause of hospital readmission in the U.S.
- In the U.S., sepsis is the costliest reason for hospitalization
- 20% of patients with sepsis are rehospitalized within 30 days.

Lab and Clinical Sepsis Journey
When it comes to patient care, the lab is one of the foundational hospital departments that impact patients from arrival to discharge. And with so many potential touch points, there’s an opportunity to improve patient outcomes.
Webinar Supporting Patient Sepsis Journeys from the Lab
Watch Dr. Tobin Efferen and Hunter Bowen’s presentation on sepsis diagnosis and management highlighting the use of standardized laboratory and clinical operations in the context of one patient’s journey from initial assessment in the Emergency Department through treatment in the Intensive Care Unit to eventual discharge.

Infographic Solutions that Impact Sepsis Patient
With increasing frequency, UTIs caused by ESβL-producing Enterobacterales are seen in outpatients with no previous healthcare exposures.5 Learn more about how our MicroScan panels feature drugs recommended by IDSA* and the ECDC** to treat pyelonephritis and complicated urinary tract infections caused by ESBLs.

Clinical Lab Solutions to Provide Valuable Diagnostic Insights
-
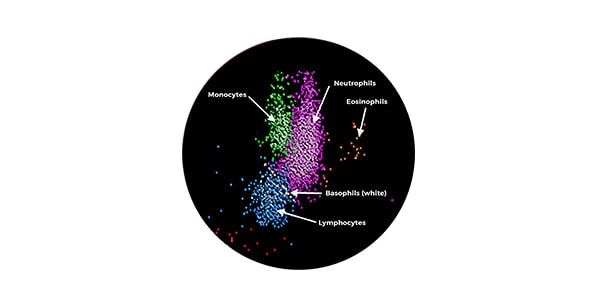
Hematology
Find out more -

Immunoassay
Find out more -

Urinalysis
Find out more -
Microbiology
Find out more
Proud Sponsor
*IDSA- Infectious Disease Society of America
**ECDC- European Centre for Disease Prevention and Control
1Faisal, M., et al. (2019). Computer-aided National Early Warning Score to predict the risk of sepsis following emergency medical admission to hospital: a model development and external validation study. Canadian Medical Association Journal, 191(14), E382–E389. https://doi.org/10.1503/cmaj.181418
2https://www.globaldata.com/store/report/severe-sepsis-and-septic-shock-epidemiology-analysis/
3Jones SL et al. “Reductions in Sepsis Mortality and Costs After Design and Implementation of a Nurse-based Early Recognition and Response Program.” Jt Comm J Qual Patient Saf, vol. 41, no. 11. 2015, pp. 483–91
4Judd WR, Stephens DM, Kennedy DA. “Clinical and Economic Impact of a Quality Improvement Initiative to Enhance Early Recognition and Treatment of Sepsis.” Ann Pharmacol, vol. 48, no. 10. 2014, pp. 1269–75
5. CDC. 2019. Antibiotic Resistance Threats in the United States; https://www.cdc.gov/drugresistance/biggest-threats.html#extend
 English
English




